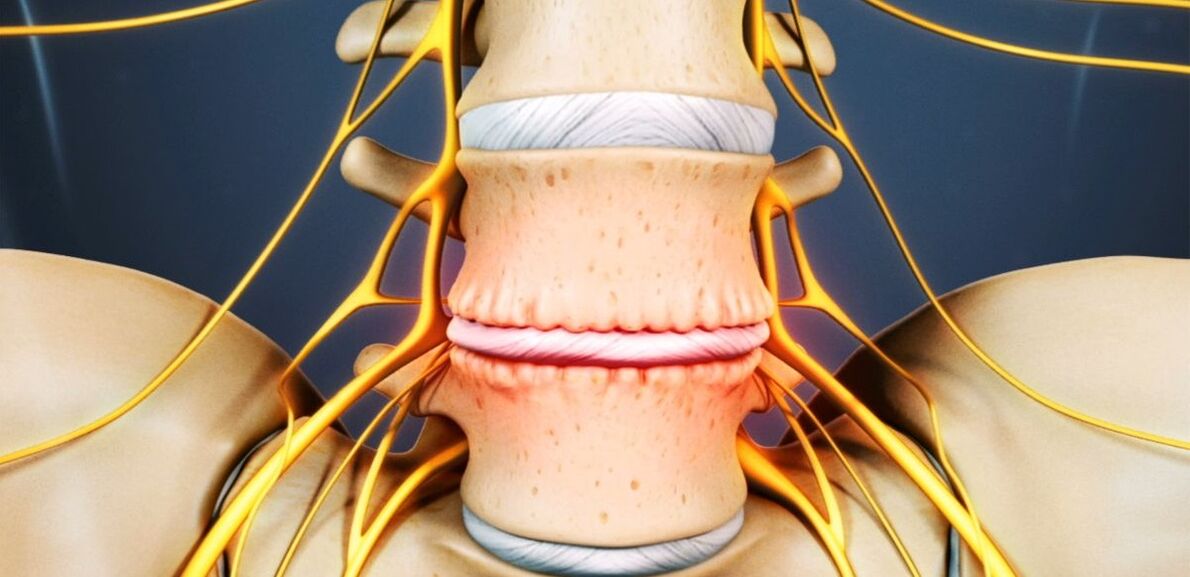
Osteochondrosis is a chronic degenerative-dystrophic disease that develops under the influence of many quite different factors. Initially, pathological changes occur in the nucleus pulposus (internal contents of the intervertebral disc), and then spread to the fibrous ring (outer shell of the disc) and other elements of the spinal movement segment (SDS). This can be a consequence of the natural aging process of the body, or it can occur in the background of injuries, increased load on the spine and other causes. In any case, osteochondrosis is only the first stage of destruction of the intervertebral disc, and if left untreated, protrusions and hernias occur that often require surgical removal.
The intervertebral disc is a cartilage formation that separates the vertebral bodies and acts as a shock absorber.
Osteochondrosis of the lumbar region: what is it
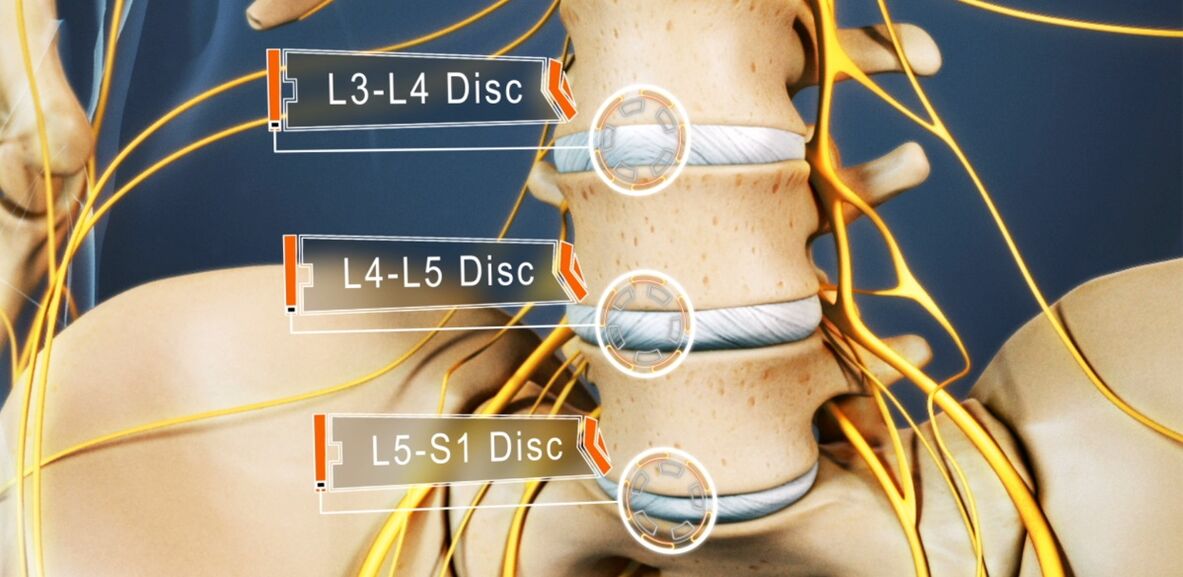
48 to 52% of people suffer from osteochondrosis. And osteochondrosis of the lumbar spine is the most common. The disease can affect any of the intervertebral discs of the lumbosacral spine, several of them, or even all of them. Disks L5-S1, L4-L5 suffer most often, L3-L4 less often. The upper lumbar discs (L3-L2 and L2-L1) are much less commonly affected.
The prevalence of lumbar osteochondrosis is due to the fact that the greatest load in performing any physical work, especially lifting and carrying weights, walking, running, sitting, falls on the lower back. The lumbar spine consists of 5 vertebrae, which are much larger than the thoracic and cervical vertebrae. Accordingly, the intervertebral discs that separate them are larger in size. Normally, the lumbar region has a slight anterior curvature (physiological lordosis). It is the last moving part of the spine and is located next to the fixed sacrum, so lumbosacral osteochondrosis is most commonly referred to.
If before osteochondrosis was considered an age-related disease, today its first manifestations can be seen as early as 15-19 years of age. Among 30-year-olds, 1. 1% of people already suffer from severe symptoms of degenerative-dystrophic changes on the intervertebral discs. And in the representatives of the older age group (from 59 years), the clinical manifestations of the disease are already present in 82. 5%. At the same time, the incidence of pathology continues to rise steadily, largely due not only to an increase in the average age of the country’s population, but also to lifestyle changes that are not for the better.
Reasons for development
Today, there is still no consensus on the etiology of degenerative diseases of the spine. However, the main theory of their development is involutive. According to her, osteochondrosis is a consequence of previous damage to the intervertebral disc and bone structures of the spine, as well as the appearance of inflammatory and other processes. The theory suggests that degenerative changes are genetically predisposed and are, in fact, inevitable. And their clinical manifestation, especially in young and middle-aged people, is due to the influence of various endogenous and exogenous factors.
Thus, the development of osteochondrosis of the lumbar spine is facilitated by:
- heavy physical work, especially associated with lifting heavy loads;
- sedentary, sedentary lifestyle;
- any back injuries, including bruises;
- overweight;
- metabolic disorders;
- posture violation, spinal deformity;
- flat feet and other foot pathologies;
- pregnancy, especially multiple pregnancy.

Pathogenesis
Regardless of the causes, degeneration of the intervertebral disc occurs when the intensity of the process of catabolism (cleavage and oxidation of molecules) of matrix proteins begins to exceed the rate of their formation. One of the key points in this process is the malnutrition of the intervertebral discs.
Because they, like most cartilage in adults, do not have a direct blood supply, as they are deprived of blood vessels, the influx of nutrients to them and the removal of metabolic products takes place by diffusion with successive compression and relaxation of the disc during movement. The main structure that gives power to the disk are the end plates that are located on its upper and lower surface.
By themselves, the end plates are a bilayer formed of cartilage cells and bone tissue. Accordingly, the cartilaginous side is next to the disc, and the bone - along the bodies of the vertebrae. They are characterized by good enough permeability, which ensures the exchange of substances between cells, intercellular substance of the disc and blood vessels that pass in the bodies of the vertebrae. Over the years, especially under the negative influence of external and internal factors, the structure of the end plates changes, and their blood supply decreases, leading to a decrease in the intensity of metabolism in the intervertebral disc. As a result, its ability to produce a new matrix decreases, leading to a progressive decrease in its density with age.
At the molecular level, this is followed by:
- reducing the rate of diffusion of nutrients and metabolic products;
- decreased cell vitality;
- accumulation of cell breakdown products and altered matrix molecules;
- reduction of proteoglycan production (high molecular weight compounds responsible for the formation of new cartilage cells and which are the main sources of chondroitin sulfate synthesis);
- collagen scaffold damage.
Possible consequences
As a result of ongoing changes, the intervertebral disc is dehydrated, and the nucleus pulposus loses the ability to adequately distribute the loads falling on it. As a result, the pressure inside the disc becomes uneven, so the fibrous ring experiences overload and compression in several places. Since this happens with every movement of a person, the ring is regularly subjected to mechanical pressure. This leads to negative changes in it.
Also, frequent reduction in disc height and elasticity leads to compensatory changes in adjacent vertebral bodies. Bone growths called osteophytes form on their surfaces. They tend to increase over time and even merge with each other, ruling out the possibility of a shift in the affected PDS.
Due to the fact that malnutrition causes damage to the collagen skeleton, under the influence of the pressure of the nucleus pulposus in certain places, the normal structure of the fibers that form the fibrous ring is disturbed. In the absence of intervention, this eventually leads to cracks and fractures on them. Gradually, more and more fibers of the fibrous ring are torn at the site of application of the pressure, which leads to its protrusion. This is especially facilitated by the increased load on the spine. And since the lumbar part takes the main load during movement and any physical activity, it most often suffers.
Protrusion of the intervertebral disc without final rupture of the fibrous ring and with the size of its base larger than the protruding part is called protrusion. With a complete rupture in one place or another, an intervertebral hernia is diagnosed.
By destroying part of the fibers of the fibrous ring, the pressure in the disk gradually decreases, leading to a reduction in tension and the fibers themselves. This leads to a violation of its fixation and, as a result, pathological mobility of the affected segment of the spine movement.
The vertebral motor segment (SMS) is a structural and functional unit of the spine made up of the intervertebral disc, adjacent vertebral bodies, their facet joints, ligaments, and muscles attached to these bone structures.
Normal functioning of the spine is possible only with the proper functioning of the PDS.
Symptoms of lumbar osteochondrosis
The disease can be asymptomatic for a long time, and then begins to manifest itself as a slight discomfort in the lumbar region, which gradually becomes effective. But in some cases, osteochondrosis of the lumbar part begins acutely, immediately causing a strong pain syndrome. In most cases, the signs of pathology first appear after 35 years.
Back pain is the main symptom of the disease. It can be of different character and be painful and dull, acute, constant or episodic. But at the base of the pathology, especially in the early stages of development, is characterized by a change in the period of exacerbation and remission, and hypothermia or lifting a heavy object, or unsuccessful, sudden movement can cause another deterioration in well-being.
The pain is often accompanied by a feeling of numbness and tension in the back muscles. They are intensified by physical exertion, sudden movements, lifting heavy loads, bending, and even coughing and sneezing.

If, due to the instability of the vertebral body, the root of the nerve that extends from the spinal cord is tightened by one or another anatomical structure, this will lead to the development of appropriate neurological disorders. Their main manifestations are:
- cracking, severe pain radiating to the sacrum, buttocks, lower limbs, or perineum;
- sensitivity disorders of varying severity;
- mobility restrictions, lameness;
- weakness in muscles innervated by a pinched nerve.
In the lumbar spine, the spinal cord ends at the level of 1-2 vertebrae and passes into the so-called cauda equina, formed by the accumulation of spinal roots. Moreover, each of them is responsible not only for the innervation of the muscles, but also for certain organs of the small pelvis, so prolonged compression can cause disturbances in the work of the corresponding organ. This can lead to the development of impotence, infertility, gynecological diseases, hemorrhoids and other disorders.
The clinical picture of osteochondrosis of the lumbar spine, especially with a long course and the appearance of compression of the spinal roots, largely depends on the level of the lesion, ie on which disc has undergone degenerative-dystrophic changes.
- Defeat of the L3-L4 disc - pain is given in the front-inner parts of the thigh, lower leg and inner ankle. This is accompanied by a decrease in the sensitivity of the anterior thigh surface, a decrease in strength or loss of knee twitch, as well as a decrease in the strength of the quadriceps muscles.
- Defeat of the L4-L5 disc - pain is given from the upper part of the buttocks to the outer parts of the thigh and lower leg. Less commonly, this is accompanied by the spread of pain to the back of the foot, including 1-3 toes. There is a decrease in muscle sensitivity and weakness in these areas. Hypotrophy and incomplete extension of the big toe sometimes develop.
- L5-S1 disc damage - pain begins in the middle zone of the buttocks and descends to the heel along the posterior or posterior surface of the thigh and lower leg and can affect the outer edge of the foot, such as 4-5 toes. Sensitivity decreases in these areas of the lower extremities, and gastrocnemius and gluteus maximus often decrease in size, which is accompanied by their weakness. If the spinal root is affected, which passes at the level of this PDS, a decrease or loss of Achilles and plantar reflexes can be noticed.
Disks L1-L2 and L2-L3 are rarely affected.
The pain that accompanies the disease limits the person and significantly reduces the quality of his life. Since they last for a long time and are repeated regularly, if not constantly present, it cannot but affect the psycho-emotional state. As a result, more than half of patients show signs of chronic emotional stress, depressive disorders, etc.
Diagnosis
If there are signs of osteochondrosis of the lumbar spine, you should contact a neurologist or vertebrologist. First of all, the doctor collects the anamnesis, which consists in clarifying the nature of the complaints, the characteristics of the pain, the conditions for their occurrence and reduction, the characteristics of the person's working life, etc.
The second phase of the diagnosis, which is carried out within the first consultation with the doctor, is a physical examination. During it, the doctor assesses the condition of the skin, posture, the depth of the physiological curves of the spine, the presence of its curvature, etc. It is obligatory to assess the condition of the muscles that surround the spine, called paravertebral, because they are often painful and overstretched, which is a reflex reaction of the body to inflammation and discogenic pain.
Based on the data obtained during the examination and examination of the patient, the neurologist may suspect the presence of osteochondrosis of the lumbar spine. But in order to exclude possible concomitant pathologies, as well as to confirm the diagnosis and precisely determine the degree of damage, the severity of degenerative-dystrophic changes on the intervertebral disc and involvement of bone structures, laboratory and instrumental diagnostic methods are needed.

Laboratory diagnostics
Different analyzes are not decisive in the diagnosis of lumbar spine osteochondrosis. They are more focused on assessing the degree of the inflammatory process and detecting concomitant disorders.
Therefore, they can be assigned:
- UAC;
- OAM;
- blood sugar test;
- blood chemistry.
Instrumental diagnostics
It has been shown that all patients with suspected osteochondrosis of the lumbar spine have:
- X-ray of the lumbar spine in two projections - allows you to determine the structure of bone structures, detect anomalies, formed osteophytes, changes in facet joints, etc. ;
- CT - allows you to detect changes in bone structures in the earlier stages of development from X-rays, as well as identify indirect signs of osteochondrosis;
- MRI is the best method for diagnosing pathological changes in cartilage formations and other soft tissue structures, which allows the detection of even the smallest changes in intervertebral discs, ligaments, blood vessels and spinal cord and accurately assess their severity and potential risks.

In addition, it may be recommended:
- densitometry - a method for determining bone density, which allows the diagnosis of osteoporosis, which is especially common in the elderly;
- myelography - allows the assessment of the condition of the CSF pathways of the spinal cord and the degree of damage to the protruding disc, which is especially important in the presence of an already formed intervertebral hernia of the lumbar spine.
Treatment of lumbar osteochondrosis
When diagnosing osteochondrosis, as a rule, all patients are initially prescribed conservative therapy, provided that there is no pronounced and progressive neurological deficit. But her character was chosen strictly individually.
Since the disease is chronic and the regenerative possibilities of intervertebral discs are extremely limited, especially in severe degenerative-dystrophic changes, the main goals of therapy are to stop their further progression and eliminate the symptoms that disturb the patient. Therefore, treatment is always complex and includes:
- drug therapy;
- manual therapy;
- physiotherapy;
- exercise therapy.
In the acute period, patients are shown to limit physical activity or even adhere to bed rest for 1-2 days. This will help relax the muscles and reduce the pressure inside the disc. If you need to sit, walk, or do physical work for a long time, you should wear a stabilizing lumbar corset.

After the end of the acute period and during the remission of the disease, on the contrary, it is important to move as much as possible, but carefully and excluding increased stress on the lower back. Patients will need to acquire the skills of proper sitting, lifting objects off the floor, carrying heavy loads, as all of this affects the course of the pathology. It is important to avoid tilting and sudden movements, lifting something off the floor or low surfaces, after bending the knees, not bending. Sit only with your back straight on a chair that supports your back well. In addition, during sedentary work, it is important to take regular breaks for short training. It is important to avoid falls, jumps, fast running and hypothermia.
In osteochondrosis, it is important to maintain body weight within optimal limits, and obesity is indicated diet and exercise appropriate to the patient's condition, because excess weight creates an increased load on the lower back and causes faster progression of pathological changes in the discs.
On average, conservative therapy is usually designed for 1-3 months, although it can take longer. But even after completing the main course prescribed by your doctor, you will need to continue taking a range of medications, exercise therapy, and adhere to lifestyle recommendations.
Medical therapy
The main components of drug therapy are individually selected drugs from the NSAID group. When choosing them, the doctor takes into account not only the severity of the pain syndrome and the course of the inflammatory process, but also the nature of concomitant diseases, especially digestive tract, because NSAIDs with prolonged use can adversely affect the condition of their mucosa and cause exacerbation of various pathologies.
It is necessary to use NSAIDs for acute lower back pain, immediately after their onset. Preferably in 1-2 days. Depending on the severity of the patient's condition, they can be administered intramuscularly, in the form of rectal suppositories, topical agents and in oral forms. The duration of admission should not exceed 2 weeks. In the future, an individually selected drug is taken on demand, but trying to avoid frequent use.
Recently, drugs, which include selective cyclooxygenase-2 inhibitors, have become increasingly preferred.
Also, patients are prescribed drugs of the following groups:
- muscle relaxants - help to relax overly tense muscles and thus reduce back pain;
- chondroprotectors - improve the course of metabolic processes in the intervertebral disc (especially effective when they begin in the earliest stages of development of lumbar osteochondrosis);
- B vitamins - contribute to the improvement of nerve conduction;
- antidepressants and anxiolytics - are used for long-term osteochondrosis, which has led to depression, chronic fatigue and other mental disorders.
In very severe pain, especially of neurological origin, therapeutic blockades are performed. They involve the introduction of anesthetics in combination with corticosteroids at points near the compressed nerve, leading to rapid pain relief. But the procedure can be performed only in a medical institution by specially trained health workers, because it is associated with the risk of complications.
Manual therapy
Manual therapy allows not only to improve the quality of blood circulation in the affected area, but also to significantly reduce the severity and duration of pain in osteochondrosis. It effectively relieves muscle tension and allows you to remove functional blocks, which significantly increases the mobility of the affected SMS.
Also, with well-conducted manual therapy, it is possible not only to increase the distance between the vertebrae, return them to the anatomically correct position, but also to release the compressed nerve roots. As a result, the pain is quickly eliminated and the neurological disorders disappear. It also reduces the likelihood of complications and disorders in the work of internal organs.

Additional positive properties of manual therapy are improving mood, strengthening immunity, activating the body's natural recovery mechanisms and increasing efficiency. Usually after the 1st session there is a noticeable improvement in well-being, and in the future the effect becomes even more pronounced. As a rule, the course consists of 8-15 sessions, and it is important to complete it by the end, even with complete normalization of well-being.
Physiotherapy
After calming the acute inflammation, courses of physiotherapeutic procedures are indicated, which not only help to reduce pain, but also improve microcirculation, nutrition and the course of reparative processes in the area of degenerative-dystrophic changes. Patients are usually prescribed:
- drug-induced electrophoresis;
- electrical neuromyostimulation;
- ultrasound therapy;
- laser therapy;
- magnetotherapy;
- UHF.
Which specific methods of physiotherapy will give the best effect, the frequency of their application, the duration of the course and the possibility of combining it with other types of exposure are determined individually for each patient.

Traction therapy gives very good results in osteochondrosis of the lumbar spine. Thanks to it, it is possible to achieve an increase in the distance between the vertebral bodies, which currently reduces the load on the affected discs. After the session, in order to consolidate the results, the patient must wear an orthopedic corset.
exercise therapy
After the elimination of acute pain, the treatment program must be supplemented with exercise therapy. Its main tasks are stretching the spine and relaxing the cramping muscles of the lower back. Also, therapeutic exercises help strengthen the muscular corset, create reliable support for the spine and improve posture. This inevitably activates blood circulation and improves metabolic processes, which has a beneficial effect on the nutrition of the discs.
A set of exercises is individually selected for each patient in accordance with the degree of degenerative-dystrophic changes, the degree of physical development of the patient, the nature of the accompanying disorders, age and other factors. Initially, learning under the guidance of an experienced therapy exercise instructor is recommended.
All patients with degenerative changes of the spine are recommended to visit the pool 2-3 times a week, because swimming lessons minimize the load on the spine, but allow you to effectively strengthen the back muscles.
Therefore, osteochondrosis of the lumbar spine is one of the most common diseases. At the same time, it can deprive a person of working ability for a long time, and even lead to disability due to the development of complications. Therefore, it is important not to ignore the first symptoms of the disease, when it is easiest to deal with it. With the appearance of pain, and even more numbness, limited mobility, back pain, it is necessary to contact a neurologist as soon as possible, undergo the necessary examination and begin treatment. In this case, it will be possible to stop the pathological process and return to a normal, full life without pain and significant limitations.

























